Malaria: Asexual & Sexual Life Cycle , Lab Diagnosis
Malaria is one of the most widely spread parasitic disease of the world. It mainly occurs in tropical and subtropical areas but cases are found all over the world due to travelling to and from these areas. A protozoan belonging to the class sporozoa and the genus plasmodium causes it. Four species are involved namely, P.vivax, P.ovale and P.falciparum. All species differ in morphology, life cycle and type of diseases they cause. The parasite in invades and destroys red blood cells. It is transmitted from one person to another through bites of a mosquito of the genus anopheles.
Life Cycle:
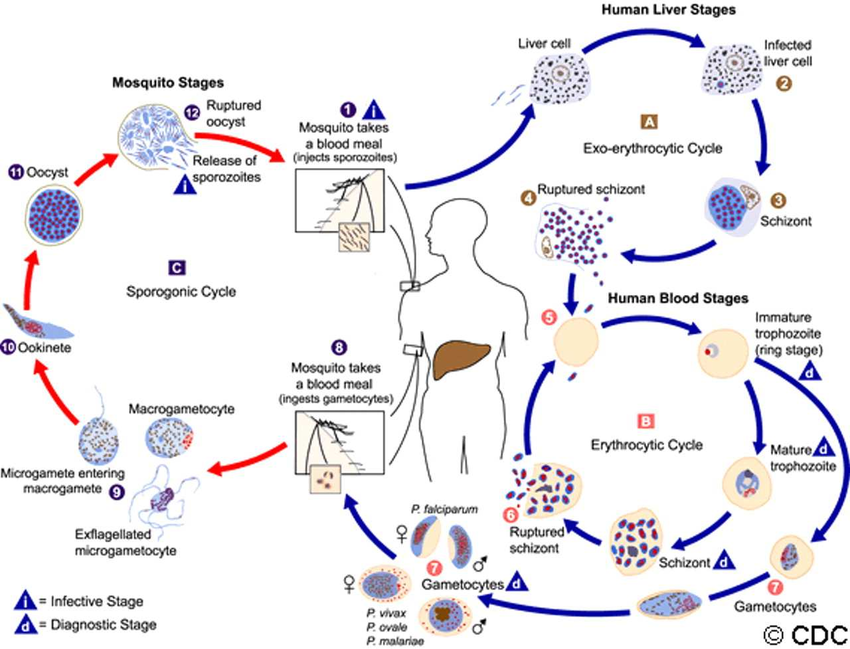
Life cycle of malaria parasite involves two host and consists of a sexual cycle or sporogony in mosquito and asexual cycle or schizogony in man. Man is actually the intermediate host while mosquito is the definitive host.
Asexual Cycle (Schizogony)
During a blood meal a malaria-infected female Anopheles mosquito inoculates sporozoites into the human host. Sporozoites infect liver cell and mature into schizont, which rupture and release merozoites. This is pre-erythrocytic schizogony or tissue phase. (Of note, in P.vivax and P.ovale is s dormant stage [hypnozoites] that can persist in the lives and cause relapses by invading the blood stream weeks, or even years later also called as (exoerythrocytic stage). After this initial replication in the live, the parasites undergo asexual multiplication in the erythrocytes (erythrocytic schizogony). Merozoites infect red blood cells. The ring stage trophozoites mature into schizont, which rupture releasing merozoites.
When the infection is well established, some merozoites differentiate into sexual erythrocytic stages (gametocytes) after about 12 days. Blood Stage parasites are responsible for the clinical manifestations of the disease. The length of erythrocytic cycle and the number of asexual generations varies depending upon the species. If large number of red cells rupture simultaneously, a malarial paroxysm results from the toxic materials released into the bloodstream. This time taken to complete this cycle varies in different species. In P.vivax it is 45 hours, in P.oval 48 hours, in P.malariae 72 hours and P.falciparum 48 hours. Fever occurs at the time of liberation of merozoites.
Sexual Cycle:
The sexual forms of the parasite the gametocytes, male (microgametocytes) and female (macrogametocytes), are ingested by an Anopheles mosquito during a blood meal. The parasites multiplication in the mosquito is known as sporogony. While in the mosquito’s stomach, the microgametes penetrate the macrogametes generating zygotes. The zygotes in turn become motile and elongated (ookinetes), which invade the midgut wall of the mosquito where they develop into oocysts. The oocysts grow, rupture and release sporozoites, which make their way to the mosquito’s salivary glands. Inoculation of the sporozoites into a new human host prepetuates the malaria life cycle. All sexual and asexual forms of the parasite described in human cycle are seen in peripheral blood except in P.falciparum where most of maturation occurs in RBCs sequestered in small vessels. In this case only ring forms and gametocytes are seen in the blood. It is important to identify and report P.falciparum because it not only gives rise to immediate serious complications but may also be resistant to ordinary drugs. The incubation period varies from 8-11 days in P.falciparum to 18-40 days in P. malariae. However somtimes it may be prolonged for months to years.
Laboratory Diagnosis:
The diagnosis depends upon demonstration of the parasite in blood. Thick smear is used as a screening test, whereas the thin smear is to identify the species. Two Stains are uses. Leishman stain is prepared in alcohol which also act as fixative, so both fixation and staining occur at the same time. On the other hand, in Giemsa staining the fixative and stain are separate, thus the thin film must be fixed prior to staining. Fluorescent dye may also be used, but this employs the use if fluorescence microscope. The immunodiagnostic procedures include indirect fluorescent antibody technique, indirect haemagglutination and parasite DNA detection by PCR but are not used in routine. The best time for collection of a blood sample is 6-12 hours after the onset of a chill as the blood at this time will contain larger number of trophozoites. It sholud be repeated 8 hours later to see matire trophozoites that are species specific. It is best to use fresh non-coagulated capillary blood, obtained by a prick.