URINALYSIS: PHYSICAL EXAMINATION & INTERPRETATION
In Urinalysis, Urine physical examination is a fundamental component of medical diagnostics and clinical assessment, offering valuable insights into an individual’s overall health and hydration status. This non-invasive and cost-effective procedure involves a comprehensive evaluation of various visual and physical characteristics of urine, providing healthcare professionals with essential data to identify potential health issues or monitor a patient’s condition.
By examining the Volume, Color, Odor, Appearance, pH level and relative Specific Gravity of urine, clinicians can gather valuable information about a patient’s hydration level, kidney function, and the presence of certain substances or abnormalities in the body. Furthermore, measuring the volume of urine produced over a defined period helps in assessing urinary system functionality.
Urine physical examination serves as an essential tool in diagnosing and managing a wide range of medical conditions, from kidney diseases and urinary tract infections to metabolic disorders and dehydration. This introductory step in the diagnostic process lays the foundation for more targeted medical investigations and plays a crucial role in maintaining and improving patient health. In this context, we will explore the key components and significance of urine physical examination in greater detail.
Volume:
Urine volume can vary depending on several factors, including an individual’s hydration status, diet, activity level, and overall health. Here are some common categories of urine volume:
1. Normal Urine Volume
The average person typically produces between 800 milliliters (mL) and 2.5 liters (L) of urine per day. This range can vary depending on factors such as age, sex, and individual differences. A normal daily urine output is around 1 to 2 liters for most adults.
2. Polyuria
Polyuria is a condition characterized by the production of abnormally large volumes of urine. It can be caused by various factors, including excessive fluid intake, diabetes mellitus (high blood sugar levels), diabetes insipidus (a condition affecting water balance in the body), certain medications, and kidney disorders.
3. Oliguria
Oliguria is the production of a reduced amount of urine, typically less than 400 mL per day. It can be a sign of dehydration, kidney disease, urinary tract obstruction, or other medical conditions.
4. Anuria
Anuria is the absence of urine production or an extremely minimal urine output, usually less than 100 mL per day. It is a medical emergency and can result from severe kidney failure, urinary tract obstruction, or other critical conditions.
5. Nocturia
Nocturia refers to the need to wake up and urinate frequently during the night. It can be caused by a variety of factors, including age-related changes in bladder function, an overactive bladder, or certain medical conditions.
6. Diurnal variation
Diurnal variation in urine volume refers to the natural variation in urine output throughout the day. Generally, urine production is highest during the day and decreases at night. This variation is influenced by factors such as fluid intake, body position, and hormonal fluctuations.
7. Stress-induced diuresis
Stress or intense physical activity can lead to increased urine production due to the release of stress hormones like cortisol and adrenaline. This can cause a temporary increase in urine volume.
8. Fluid overload
When a person consumes an excessive amount of fluids in a short period, it can lead to an increase in urine volume as the body attempts to eliminate the excess fluid. This can be seen in conditions like water intoxication.
Odor:
Odor in urine can vary based on a person’s diet, hydration level, and health conditions. Here are some common types of odor in urine and their potential causes:
1. Ammonia-like Odor
This can be a normal smell, especially if you have consumed foods rich in nitrogen, such as asparagus, or if your urine is concentrated due to dehydration. However, it can also be a sign of a urinary tract infection (UTI).
2. Sweet or Fruity Odor
This odor might indicate uncontrolled diabetes, as excess sugar in the bloodstream can be excreted in the urine.
3. Musty or Fishy Odor
This odor can be a sign of a metabolic disorder called phenylketonuria (PKU), in which the body can’t break down an amino acid called phenylalanine properly.
4. Strong Medicinal Odor
Some medications, such as antibiotics, can cause urine to have a strong and distinct odor.
5. Sulfur or Rotten Egg Odor
This might be due to the breakdown of sulfur-containing proteins in certain foods, or it could be related to a gastrointestinal issue.
6. Maple Syrup Odor
A sweet, maple syrup-like odor in urine can be a sign of maple syrup urine disease, a rare genetic disorder.
7. Foul or Offensive Odor
A foul odor can be indicative of a urinary tract infection, a bladder infection, or other health issues. It’s important to seek medical attention if you notice a persistently foul odor.
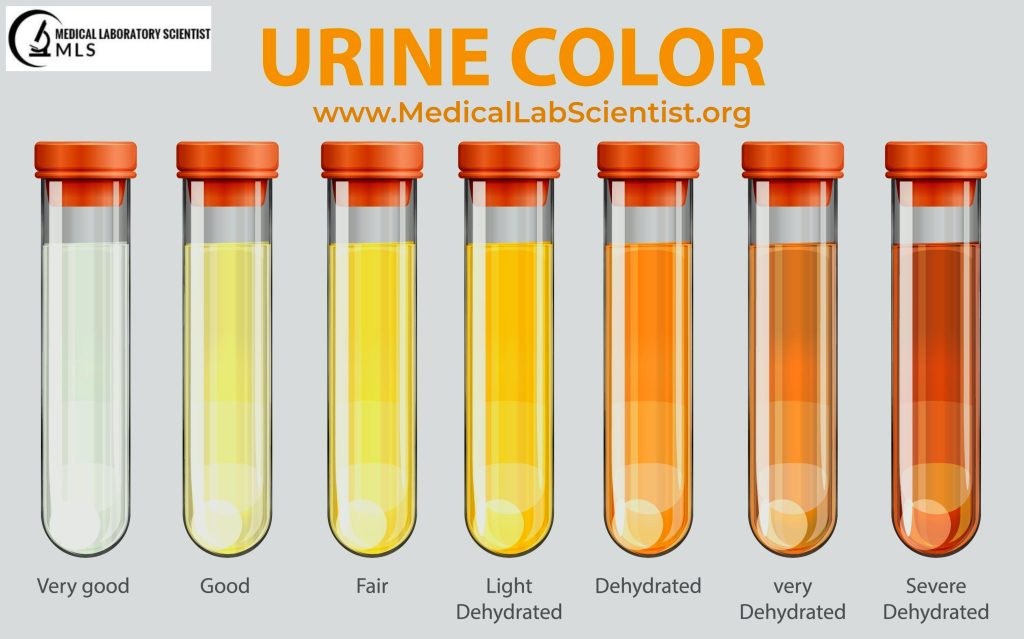
Color:
The color of urine is typically pale yellow due to the presence of pigments like uroerythrin, urochrome, and porphyrins. The color can vary with specific gravity and may become deep orange in highly concentrated urine. Urine color can also change due to certain diseases, as well as consumption of specific foods, food dyes, and medications. It’s important to consider the influence of drugs on urine color before making any interpretations.
Color of Urine and Possible Causes:
Urine color can vary widely depending on several factors, including your hydration level, diet, medications, and underlying health conditions. Here are some common colors of urine and what they might indicate:
1. Pale Yellow to Straw-colored Urine
This is the most common and normal urine color. It indicates that you are well-hydrated and your body is functioning normally.
2. Dark Yellow to Amber Urine
Darker yellow urine may simply be a sign of dehydration, suggesting that you need to drink more water. However, it can also result from certain foods, vitamins, or medications.
3. Orange Urine
Urine that appears orange can result from the consumption of foods like carrots or beets or from medications containing certain dyes. It can also be due to dehydration. In some cases, orange urine may indicate a liver or bile duct problem.
4. Brown or Tea-Colored Urine
Brown or tea-colored urine may be a sign of liver disorders, such as hepatitis, or it could be related to muscle breakdown (rhabdomyolysis), certain medications, or the presence of blood.
5. Pink or Reddish Urine
Pink or reddish urine can result from eating foods like beets, blackberries, or rhubarb, but it can also be due to blood in the urine (hematuria). Hematuria can be caused by urinary tract infections, kidney stones, or more serious conditions like bladder or kidney cancer.
6. Green or Blue Urine
Although rare, green or blue urine can occur as a result of consuming certain foods or medications. It is typically harmless but should be investigated if it persists and is not linked to dietary factors.
7. Cloudy Urine
Cloudy urine may be caused by the presence of minerals, crystals, or cells in the urine. It can be a sign of a urinary tract infection, kidney stones, or other medical conditions. In some cases, it may be normal and related to dietary factors.
8. Foamy Urine
Foamy urine can be a normal variation and may not necessarily indicate a problem. However, persistent foamy urine could be a sign of excessive protein in the urine (proteinuria), which may be associated with kidney disease.
9. Purple or Violet Urine
Purple or violet urine is very rare and is usually the result of specific medications or foods. It is typically not a cause for concern.
Appearance:
Freshly voided urine should be clear, but it may become cloudy upon standing due to the presence of various substances like phosphates, urates, oxalates, pus, bacteria, fat, and chyle.
pH:
Urine pH measures the hydrogen ion concentration and can be a useful screening test in renal diseases, respiratory diseases, metabolic disorders, and some therapeutic treatments. Normal urine pH is acidic, ranging from 5.0 to 6.5. However, the kidneys can adjust the pH over a wider range (4.6 to 8.0, with a mean of 6.0).Urine pH can be assessed using indicator paper or strips that contain methyl red (red strips) and bromothymol blue (blue strips), providing a pH range of 5.0 to 9.0. To test pH, a strip is dipped in urine, excess urine is allowed to drain off by touching the edge of the container, and then the color is compared to a reference chart.
- Acid: pH <7.0 (blue litmus changes to red).
- Alkaline: pH >7.0 (red litmus changes to blue).
- Neutral: pH 7.0 (No change of color in both the litmus).
- Amphoteric (buffered): When both the litmus shows color change.
Alkaline pH is observed in Bacterial decomposition of urine at room temperature can result from various factors, including bacterial infection, physiological alkaline tide, a vegetarian diet, certain drugs, renal failure, pyloric obstruction, vomiting, and metabolic alkalosis. Additionally, an alkaline pH of urine can be observed in urinary tract infections (UTIs) caused by urea-producing organisms.
Specific Gravity:
Specific gravity is an important parameter in urine analysis and can provide valuable insights when interpreted alongside other test results. The reference range for urine specific gravity typically falls between 1.010 and 1.025. In early morning urine specimens, it may be around 1.020. Specific gravity tends to be lower in conditions such as kidney diseases, abnormal antidiuretic hormone excretion, and in newborn babies (ranging from 1.002 to 1.004). Conversely, it can be elevated in situations like dehydration, fever, and vomiting. It’s important to note that certain contrast agents used in medical procedures can interfere with conventional specific gravity measurements. Therefore, urine should be collected either before the administration of contrast medium or at least two days after its use. Colorimetric methods for specific gravity measurement are not affected by contrast agents. Specific gravity may exceed 1.050 when calculated using a urinometer.
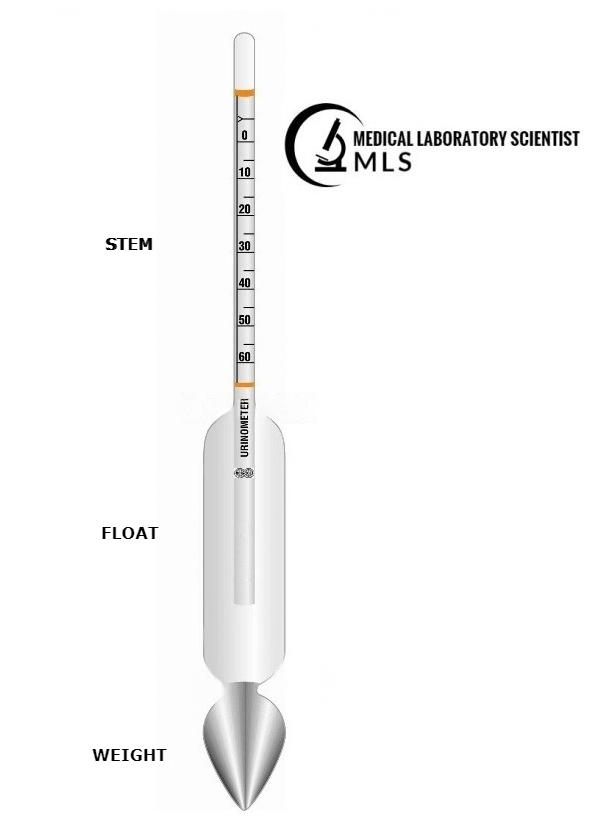
Determination:
Specific gravity can be determined using different methods, including a urinometer, refractometer, or automated equipment. When using a urinometer, the urine is allowed to equilibrate to room temperature and is thoroughly mixed. The urinometer tube is filled with urine, and the urinometer is floated in it. The specific gravity is read at the lower meniscus and should be corrected for temperature, as most urinometers are calibrated at 20°C.

Typically, for each 3°C change in temperature, a correction of 0.001 is added or subtracted. It’s important to consider the presence of substances like protein and glucose in the urine, as they can affect specific gravity. Specifically, for each 1% increase in protein content, the specific gravity increases by 0.003, while for each 1% increase in glucose content, it increases by 0.004. In cases where these substances are present, the specific gravity should be adjusted accordingly.
A specific gravity exceeding 1.020, known as hyperesthenuria, is often seen in conditions characterized by reduced fluid intake, fever, dehydration, and intravenous administration of albumin. Conversely, a specific gravity below 1.009, referred to as hypoesthenuria, is observed in situations of increased fluid intake, hypothermia, alkalosis, progressive renal failure, and sickle cell anemia. A fixed specific gravity at 1.010 may indicate chronic renal failure or end-stage kidney disease.